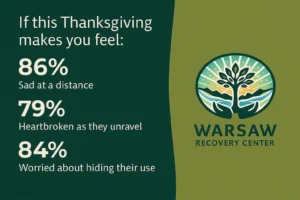
If the thought of Thanksgiving this year fills you with quiet dread, you’re not alone.
You’re trying to stay hopeful—trying to picture a peaceful holiday table, laughter, maybe even a moment that feels like “before.” But deep down, you know the patterns. Your child is using again. You can see it in the way they avoid your eyes. You hear it in the missed calls, the weird stories, the flashes of someone you recognize fading behind someone you don’t.
It’s not just about the substance. It’s about the heartbreak of watching someone you love unravel while still pretending everything is fine. If you’re here, wondering how you’re going to get through Thanksgiving, this blog isn’t going to promise you it’ll all be okay. But it will give you something else: a path forward.
Inpatient treatment programs aren’t just for rock-bottom emergencies. They’re for families like yours—families who are hurting, scared, and trying to hold onto hope when it feels like everything’s falling through their hands.
This Isn’t Your Fault—Even If It Feels Like It
Let’s say this first and say it clearly: You didn’t cause this.
You didn’t fail. You didn’t miss a warning sign that would have changed everything. You didn’t create this situation by setting a boundary—or by not setting one. Addiction has a way of warping everything around it, including your own self-perception. You start second-guessing every parenting decision you’ve ever made.
But here’s the truth: You’re here now. You’re still trying. You’re still showing up for your child even when it’s gut-wrenching and confusing and thankless. That matters more than any perfect response ever could.
And even if this isn’t the first time they’ve relapsed or struggled—you still get to try again. So do they.
What an Inpatient Treatment Program Actually Offers
Many parents picture inpatient treatment as a cold, clinical place. Stripped of warmth. Too serious. Too final. Something to avoid unless it’s the absolute last resort.
But good treatment isn’t about punishment or isolation—it’s about giving someone the space, tools, and support to interrupt the cycle they can’t break alone.
At a facility like Warsaw Recovery Center, here’s what inpatient treatment really includes:
- Medical and emotional stabilization. Withdrawal, if needed, is managed safely. Emotional dysregulation is treated with compassion, not blame.
- Therapy that meets them where they are. Not one-size-fits-all lectures. Individual therapy, group sessions, and evidence-based approaches are tailored to what they’re carrying.
- A supportive, structured environment. Daily routines help rebuild a sense of safety and purpose.
- Distance from harmful dynamics. Sometimes the healthiest thing a family can do is pause the chaos. Treatment creates a buffer—so healing can begin.
Inpatient care gives your child more than sobriety. It gives them a chance to remember who they are under the fog.
Why Holidays Can Be the Moment for Change
There’s something about holidays—especially family ones like Thanksgiving—that makes every wound sharper.
Maybe it’s the pressure to look like a happy family. Or the sadness of watching other families laugh freely while you’re scanning for red flags. Maybe it’s just the exhaustion of hoping that this year might be different.
And sometimes, that’s what nudges a family toward real change. Because when even the holidays don’t feel safe anymore, it’s a signal: this isn’t sustainable.
Inviting your child to consider inpatient treatment this time of year isn’t cold or disruptive—it’s an act of love. It’s saying: “You matter more than this performance. I don’t want another year of pretending we’re okay. I want to believe in better, for all of us.”
How to Talk to Your Child About Inpatient Treatment (Without Making Them Shut Down)
If you’re worried that bringing up treatment will push them away, you’re not alone.
It’s a delicate conversation. But it can be done in a way that builds connection instead of defensiveness. Here’s what might help:
1. Choose your moment carefully.
Avoid talking when they’re high, angry, or in front of others. Late night or early morning moments can offer more softness.
2. Lead with your emotions—not blame.
Try:
“I’ve been scared. I feel like I’m losing you, and I don’t know what to do anymore.”
3. Use simple, real language.
“I miss the version of you that used to light up this house.”
“I know you’re hurting. And I think it’s time we get real help.”
4. Offer the idea—not a demand.
You can say:
“I found a place—Warsaw Recovery. It’s not punishment. It’s help. I’d love for you to just look at it.”
Even if they say no, you’ve planted a seed. A seed that often grows when the pain gets loud enough to drown out resistance.
What Happens After You Say Yes
If your child agrees to enter inpatient treatment, a quiet kind of relief begins. Not because everything is suddenly fine—but because the freefall slows.
Here’s what to expect once you connect with a team like ours:
- Admissions Support: We’ll walk you through every step, including verifying insurance and logistics.
- Clinical Assessment: Our team will meet with your child to understand their needs and create a personalized plan.
- Family Communication: As appropriate, we’ll involve you in care planning and updates. You’re not left out—but you’re also not expected to carry it all.
- Next Steps After Treatment: Recovery doesn’t stop at discharge. We’ll support aftercare planning with outpatient services, sober housing (if needed), and resources for rebuilding.
You’re not signing them up for a short fix. You’re saying yes to long-haul support.
What If They Don’t Want to Go?
This is the hardest question, and maybe the one that hurts most.
Here’s the truth: you can’t force someone to heal. But you can stop protecting them from the consequences. You can speak honestly. You can set boundaries. You can say:
“I won’t let this destroy us both.”
“I will always love you. But I can’t support the version of this that’s killing you.”
Sometimes, that’s what turns the key. Not threats. Not guilt. Just a line drawn in love.
You’re Allowed to Hope—Even If You’re Tired
It’s okay to feel numb. It’s okay to feel furious. It’s okay to feel like you’ve done all this before and nothing changed.
But it’s also okay to hope again. To reach again. To believe that your child isn’t gone, just hurting.
This Thanksgiving doesn’t have to be the beginning of another painful season. It can be the beginning of something else entirely.
FAQ: Inpatient Treatment Programs for Young Adults
What is the difference between inpatient and outpatient treatment?
Inpatient treatment means your child stays onsite, 24/7, in a structured healing environment. Outpatient care allows them to live at home and attend scheduled sessions. Inpatient care is best when safety, stability, and focused support are needed.
Can I visit or talk to my child while they’re in treatment?
Yes, in most cases. Warsaw Recovery includes family support and communication when clinically appropriate. Boundaries are in place to protect healing—but we know how much connection matters.
What happens if they leave early or don’t want to stay?
We address this with care and honesty. Treatment isn’t jail. But we work closely with families and clients to help them stay long enough for real change to begin. If they leave, we’ll help you plan your next step.
Is inpatient treatment covered by insurance?
Often, yes. Our admissions team will help verify your insurance and explain what’s covered. We’ll also walk you through costs, payment plans, and other options if needed.
What happens after inpatient treatment ends?
We build a personalized aftercare plan with your child and your family. This may include outpatient treatment, sober living, continued therapy, and family support. Recovery is a process, and we stay with you.
Ready to take a brave next step?
Call (888) 511-9480 to learn more about our Inpatient Treatment Programs services in Warsaw, Virginia. You’re not failing. You’re fighting—for your child, and for your family. Let us help.